Atrial fibrillation (AFib or AF) is an abnormal heart rhythm (arrhythmia) caused by rapid, chaotic electrical impulses which originate in the heart’s upper chambers (atria). AFib causes the atria to beat faster than the lower chambers (ventricles) and results in an irregular heart rhythm. AFib causes the heart to beat ineffectively which can lead to blood clots in the heart. People with AFib have a 4-5 times increased risk of stroke. AFib also increases the risk of heart failure and other heart-related complications.
Some people with atrial fibrillation do not have any symptoms. However, many people experience a fast, chaotic heartbeat (palpitations), shortness of breath, or fatigue. These symptoms may make it more difficult for them to do their normal daily activities or affect their ability to exercise.
AFib may be intermittent (paroxysmal) or persistent. Over time, atrial fibrillation tends to occur more frequently and last longer. A person with atrial fibrillation may also have an arrhythmia called atrial flutter. Although atrial flutter is different from AFib, treatment for both arrhythmias is similar.
AFib itself is not life-threatening but it does require treatment to prevent atrial fibrillation-related complications like stroke and heart failure. If a person is symptomatic with AFib, treatment can also significantly improve quality of life. AFib treatment involves controlling the heart rate, resetting the heart to a normal rhythm, and blood-thinning medication to prevent stroke.
Try our Stroke Risk Calculator
Symptoms
Sometimes atrial fibrillation (AFib) does not cause any symptoms and other times it can cause severe symptoms. People who have atrial fibrillation symptoms may experience:
- Sensation of a racing heart or rapid pulse
- Irregular, pounding, or fluttering heartbeat (palpitations)
- Difficulty breathing or feeling short of breath
- Tiredness or decreased energy
- Weakness
- Chest pain
- Decreased exercise capacity
- Lightheadedness
See your healthcare provider for further evaluation if these symptoms occur to see if you have atrial fibrillation. If you have chest pain, seek immediate medical attention as this can be a sign that you are having a heart attack.
Types of atrial fibrillation
- Intermittent (paroxysmal atrial fibrillation): AFib that comes and goes. Episodes may go away after only a few minutes or can last for as long as a week. Paroxysmal atrial fibrillation may resolve on its own or it may require treatment.
- Persistent: AFib which is continuous for greater than 7 days. Symptomatic persistent atrial fibrillation may need to be treated with medications, cardioversion, or a procedure/surgery to reset the heart’s rhythm.
- Long-standing persistent: Atrial fibrillation which is continuous and lasts for longer than 1 year.
- Permanent: Continuous AFib that cannot be reset to a normal heart rhythm. Treatment goals with permanent atrial fibrillation are to control heart rate and prevent blood clots.
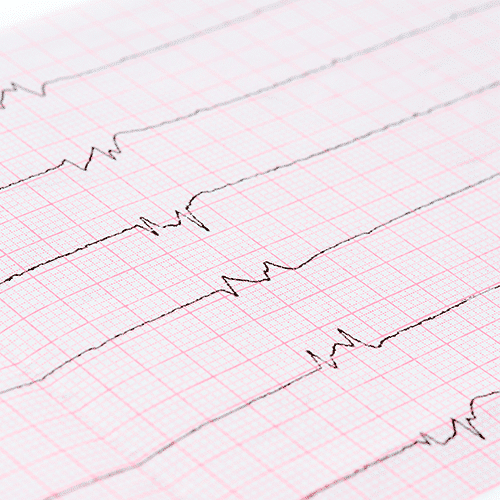
Normal Rhythm
Atrial Fibrillation Rhythm
Try our Stroke Risk Calculator
Causes
To better understand atrial fibrillation it is helpful to know how the heart normally beats.
The heart has 4 chambers: 2 upper chambers (atria) and 2 lower chambers (ventricles). The heartbeat starts in the heart’s internal pacemaker (sinus node). An electrical signal travels from the sinus node in the right atrium to the atrioventricular (AV) node, which acts as an electrical gatekeeper between the upper and lower chambers. After the electrical signal passes through the AV node, it travels throughout the ventricles. This makes the ventricles contract and pump blood through the heart and out to the rest of the body.
In atrial fibrillation, chaotic electrical signals in the atria override the sinus node. These rapid, irregular impulses make the atria quiver (shake) and ineffectively force blood to the lower heart chambers. The abnormal electrical impulses then bombard the AV node, which does its best to not to let too many signals through to the ventricles.
The resulting heart rhythm is irregular and is often too fast with a heart rate between 100-180 beats per minute. A normal heart rhythm (sinus rhythm), is steady and regular with a heart rate of 60-100 beats per minute. When the heart rate is very fast, the heartbeats can become less effective because there is no time for enough blood to fill the lower chambers to then be pumped out to the rest of the body.
Causes of atrial fibrillation
Usually, a problem with the heart’s structure causes atrial fibrillation. Some things that can damage the heart structure are:
- Blockages in the arteries that supply blood to the heart muscle (coronary artery disease)
- Heart attack
- High blood pressure
- Heart valve disease
- Heart failure
- Sleep apnea
- Thyroid produces too much thyroid hormone (hyperthyroidism)
- Lung disease
- Blood clots in the lungs (pulmonary embolism)
- Viral infections, serious illness or pneumonia
- Heart surgery
- Stimulants like certain prescription medications, over the counter medications (i.e. cold medications), street drugs and tobacco
- Alcohol
- Heart defect that you are born with (congenital heart disease)
- Problems with the heart’s natural pacemaker (sick sinus syndrome)
Some people who develop atrial fibrillation have no history of heart problems.
More about atrial fibrillation causes.
Risk factors
Certain characteristics, health conditions, and lifestyle choices increase the risk of developing AFib. Risk factors for atrial fibrillation include:
- Age: Risk of atrial fibrillation increases significantly over age 50 and continues to go up as you age.
- Gender: Men have a higher risk of atrial fibrillation.
- Family history: Atrial fibrillation runs in some families. Having a family member with atrial fibrillation is associated with a 40% increased risk of AFib.
- High blood pressure: High blood pressure is the most common modifiable risk factor for AFib and increases the risk of atrial fibrillation by 40 to 50%. If you have high blood pressure it is important to make sure it is well controlled.
- Obesity: The risk of atrial fibrillation increases as weight increases. Obesity is associated with a 49% increased risk of atrial fibrillation.
- Sleep apnea: People with sleep apnea are 4 times more likely to develop AFib. Untreated sleep apnea makes AFib treatment less effective.
- Overactive thyroid gland (hyperthyroidism): Too much thyroid hormone can irritate the heart’s electrical system and cause AFib.
- Heart disease: Any kind of heart disease (valve disease, congestive heart failure, coronary artery disease, heart attack, heart surgery, or congenital heart disease) increases risk of atrial fibrillation.
- Diabetes: People with diabetes have a higher risk of AFib. The risk increases the longer someone has diabetes and if it is not well controlled.
- Chronic health conditions: Some chronic conditions – like chronic kidney disease and lung disease – increase the risk of atrial fibrillation.
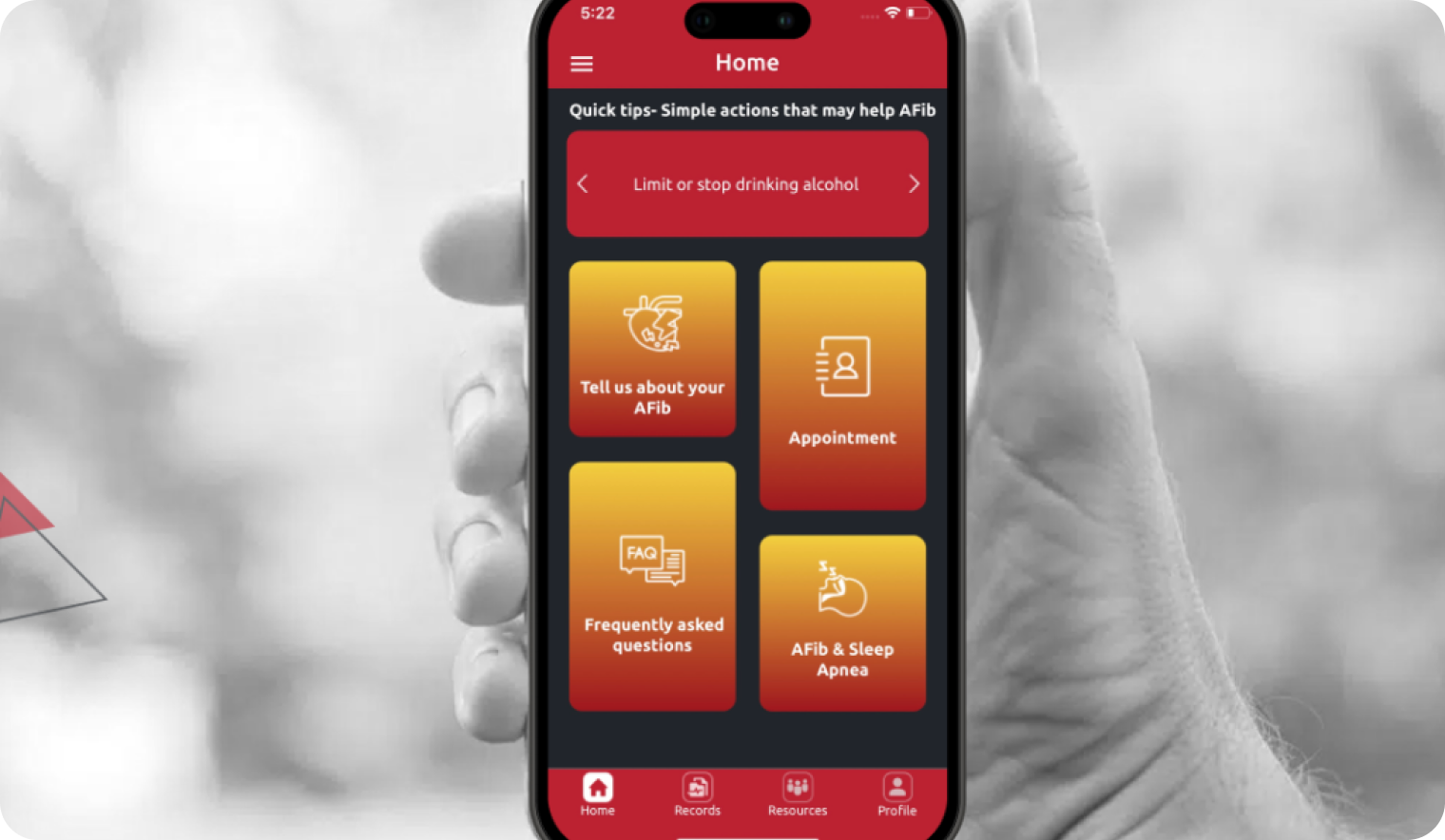
- Drinking alcohol: Excess alcohol intake and binge drinking can trigger atrial fibrillation.
- Smoking: People who currently smoke or have previously smoked have a higher risk of developing atrial fibrillation.
Try our Stroke Risk Calculator
Complications
Stroke and heart failure are the most common serious complications of atrial fibrillation.
Stroke: In atrial fibrillation, the upper chambers (atria) beat very rapidly and irregularly. This causes incomplete emptying of the atria which can allows blood to pool and form clots. If a blood clot breaks free from the left atrium it can travel to the brain, block blood flow and cause an ischemic stroke. For people with atrial fibrillation, there are certain risk factors that increase the chance of having a stroke, including:
- Increased age
- Diabetes
- High blood pressure
- Heart failure
- Underlying heart disease or history of heart attack
- History of blood clots
- Certain heart valve diseases
Blood-thinning medicine is commonly prescribed to people with AFib to prevent blood clot formation and stroke.
Heart failure: Atrial fibrillation can contribute to heart failure by various mechanisms. The most common is because AFib can cause a very rapid heart rate. The elevated heart rate puts extra strain on the heart muscle and can cause heart failure. Medications can be used to slow the heart rate to prevent or try to reverse heart failure.
Diagnosis
If you develop heart palpitations or symptoms of atrial fibrillation you should be evaluated by your doctor. However, not everyone with atrial fibrillation has symptoms and it is possible that your doctor could detect it incidentally during a physical exam. In either of these examples, further testing would be needed to diagnose atrial fibrillation. Testing may include:
- Electrocardiogram (ECG or EKG): This is the primary test for diagnosing atrial fibrillation. Sticky patches (electrodes) are placed on your skin (chest, arms, and legs). Wires connect the electrodes to a machine that creates a tracing of the heart’s electrical activity. This quick test will allow your doctor to see your heart rhythm and rate. Atrial fibrillation causes characteristic abnormal patterns of electrical activity on the electrocardiogram.
- Blood tests: Blood work will be done to check your thyroid function, electrolytes and look for other abnormalities in the blood that could cause AFib.
- Echocardiogram: This is an ultrasound of the heart. It is non-invasive. It will allow your doctor to see the heart’s structure, size and how well it is functioning.
- Heart monitors: These are small, portable devices that monitor the heart rhythm, similar to an ECG.
- Holter monitor: You wear this device for anywhere from 24 hours or longer. It monitors your heart rhythm and rate continuously while you are wearing it.
- Event monitor: Similar to a Holter monitor but it only records your heart rate and rhythm when it detects an abnormality or if you experience symptoms and push a button on the monitor. An event monitor can be worn for 30 days.
- Loop recorder: A small, implantable device. During an outpatient procedure, the skin is numbed, a small (approximately 1 inch) incision is made to the left of the breastbone and the device is slid in under the skin. A loop recorder can monitor your heart rate and rhythm for 2 to 3 years.
- Stress test: During this test, the heart is stressed using either medication or exercise. During the test information will be gathered about your heart rhythm, heart rate, and blood pressure. Sometimes images are taken of the heart before and after stress to give additional information.
- Chest x-ray: X-ray images of the heart and lungs.
Treatment
There are 4 primary goals in the treatment of atrial fibrillation:
- Control the heart rate
- Maintain a normal heart rhythm
- Prevent blood clots
- Treat underlying causes and address modifiable risk factors
Your treatment plan will depend on your AFib symptoms, the type of AFib you have and the underlying causes of your atrial fibrillation. Treatment may include medications, procedures, or surgery.
Try our Stroke Risk Calculator
Medications
Medications are used to control heart rate, maintain normal rhythm and prevent blood clots. It is important to take medications as prescribed to prevent heart failure, stroke and other heart related complications.
- Rate control: Medications, like beta blockers and calcium channel blockers, are used to slow the heart rate. These medications can also lower blood pressures so they need to be used cautiously in people with low blood pressure.
- Antiarrhythmic medications: Antiarrhythmics are used to help convert the heart rhythm from AFib back to normal sinus rhythm in what is called a pharmacologic cardioversion. They are also used to help maintain a normal heart rhythm. Antiarrhythmic drugs work primarily by changing how easily electrolytes like sodium, potassium, calcium can cross the cell membrane. Potassium channel blockers (i.e. amiodarone, sotalol, and dofetilide) and sodium channel blockers (i.e. flecainide and propafenone) are common antiarrhythmic medications. These medications tend to have a relatively high risk of side effects which can limit the ability to use them long-term.
- Blood thinners (anticoagulants): These drugs help reduce stroke risk by preventing the formation of blood clots in the heart. Traditionally, an anticoagulant called Warfarin (Coumadin, Jantoven) was used. This medication is effective at preventing clots but it has to be closely monitored with blood tests to make sure its level isn’t too high (i.e. blood is too thin – increased risk of bleeding) or too low (i.e. blood is not thin enough – increased risk of blood clots). Warfarin levels can be affected by certain foods and medications. A newer type of anticoagulant that does not require frequent monitoring and is not affected by foods or medications is now commonly used. These medications include: rivaroxaban (Xarelto), dabigatran (Pradaxa), apixaban (Eliquis), and edoxaban (Savaysa).
Procedures and Surgery for AFib
Procedures to treat atrial fibrillation may be recommended instead of, or in addition to, medications. Some procedures, like electrical cardioversion, are noninvasive.
- Electrical cardioversion: This procedure uses electricity to reset the heart to a normal heart rhythm. This is typically done as an outpatient procedure. You receive sedation prior to a cardioversion. Pads or paddles are placed on the chest wall and an electrical shock is delivered to the heart to revert it to a normal rhythm.
Other procedures are minimally-invasive, catheter-based procedures. During a catheter-based procedure, the doctor inserts a small flexible tube (catheter) into a vein in the groin. The catheter is threaded from the groin up into the heart.
- Catheter ablation: This minimally-invasive AFib ablation technique uses heat (radiofrequency energy), freezing (cryoablation), or laser to create small lines of scar tissue within the atria to interrupt the electrical signals which cause atrial fibrillation. It is primarily used to treat intermittent (paroxysmal) atrial fibrillation. AFib initially originates inside the pulmonary veins. Therefore, the area around the base of the pulmonary veins, where they attach to the left atrium, is a primary target for catheter ablation. Increasing evidence supports the use of ablation early in the course of atrial fibrillation to help maintain sinus rhythm long-term and minimize AFib’s heart related complications.
- AV node ablation: Radiofrequency or cryoablation can be used to destroy the AV node and eliminate electrical communication between the upper and lower heart chambers. As part of an AV node ablation procedure, a pacemaker is implanted and is needed for life.
- Left atrial appendage closure: The left atrial appendage (LAA) is the small sac like structure that projects off the left atrium. It is the site where most AFib-related blood clots form. For people who are unable to take blood thinners, a minimally-invasive procedure can be done to implant a small device at the opening of the left atrial appendage to seal it off and prevent blood flow communication between the LAA and the left atrium.
Surgical ablation may be recommended if a person has continuous (persistent) AFib and catheter ablation has been ineffective in maintaining normal sinus rhythm. Surgical treatment of AFib is recommended if a person with AFib is undergoing certain types of heart surgery (i.e. coronary artery bypass or valve surgery).
- Maze surgery: This type of ablation is done via a surgical approach. It is similar to a catheter AFib ablation because it also uses radiofrequency or cryoablation to create scar tissue in the heart that interrupts electrical signal pathways to prevent atrial fibrillation. It is more invasive than catheter ablation but it is more effective at treating persistent AFib and is the preferred ablation technique in those who require another type of heart surgery as well.
Atrial Fibrilation Prevention
An important thing you can do for atrial fibrillation disease control and prevention is to treat modifiable risk factors for AFib and make healthy lifestyle choices. Modifiable risk factors are underlying health conditions that can cause atrial fibrillation and include:
- High blood pressure
- Diabetes
- Obesity
- Sleep apnea
- Heart disease
- Smoking
- Excessive alcohol intake
A healthy lifestyle can prevent or improve the management of both atrial fibrillation and its modifiable risk factors. Lifestyle changes do not need to happen all at once. Making sustainable adjustments to your lifestyle over a period of time can have a significant impact on AFib, your overall health, and your quality of life.
- Eat a heart healthy diet: A diet that improves heart health is high in vegetables, fruits, beans, nuts & seeds, whole grains and lean protein and low in sugar, salt and saturated fat.
- Exercise: Moderate-intensity exercise has been shown to be beneficial for people with AFib. The American Heart Association recommends at least 150 minutes per week of moderate-intensity exercise and strength training at least 2 days per week. However, not all exercise is good for people with atrial fibrillation. There have been multiple studies which show that high-intensity endurance training can increase the risk of atrial fibrillation.
- Don’t smoke: Talk to your healthcare provider if you smoke and are considering quitting. There are numerous resources and multiple medications available to help you quit smoking.
- Limit alcohol intake: Alcohol can contribute to atrial fibrillation, especially binge drinking and chronic excessive alcohol intake. If you are going to drink alcohol, it is recommended that women drink no more than 1 drink per day and men drink no more than 2 drinks per day. Binge drinking is defined as drinking more than 4 alcoholic beverages on one occasion for women and 5 for men.
- Maintain a healthy body weight: Obesity increases the risk of atrial fibrillation and can make atrial fibrillation treatments less effective. If you are overweight or obese, losing as little as 10% of your body weight can have a significant impact on your risk of developing AFib. Read more about diet tips for Afib.
- Take medications as directed: It is important to work closely with your doctor to make sure that your underlying health conditions are controlled. See your doctors regularly, follow their advice and take your medications as directed. If you are taking a medication and have developed unwanted side effects or feel that it is not helping, follow-up with your provider. There are often many treatment options available for any given health condition.
- Manage your stress: Anger and stress can trigger atrial fibrillation. Yoga, Tai Chi, Qigong, acupuncture, meditation and counseling therapy can all be helpful stress management tools.
What to do if you think you have atrial fibrillation
If you have symptoms of atrial fibrillation, make an appointment to see your primary care provider. This will start the process to get atrial fibrillation diagnosed. If a diagnosis of AFib is confirmed, you may be referred to a heart specialist (cardiologist). A cardiologist is an expert in treating heart conditions and is best equipped to provide medical advice about managing your AFib. Getting atrial fibrillation treated early in the disease process can slow the progression from paroxysmal to persistent AFib and make atrial fibrillation treatments more effective.
Try our Stroke Risk Calculator
Sources
Zipes, D., et al. (2019). Braunwald’s heart disease: a textbook of cardiovascular medicine, 11th edition. Philadelphia: Elsevier.
National Heart, Lung, and Blood Institute. Atrial fibrillation. US Department of Health & Human Services https://www.nhlbi.nih.gov/health-topics/atrial-fibrillation. Accessed September 24, 2021
American Heart Association. American heart association recommendations for physical activity in adults and kids. https://www.heartorg/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults. Accessed September 28, 2021.
Elsevier Point of Care. Clinical overview: atrial fibrillation. https://www.clinicalkey.com/#!/content/clinical_overview/67-s2.0-bf8f83df-c155-4df0-aa76-b26e711ced71. Elsevier BV. Updated April 11, 2021. Accessed September 24, 2021.
Heart Rhythm Society. (2014). Patient information: guide to atrial fibrillation.
January, C.T., et al. 2019 AHA/ACC/HRS Focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the american college of cardiology/american heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019;140:e125-e151.
Thanks for your interest in The Scoop. Keep reading the next post to better understand the different types of AFib, and symptoms associated with each variation.