Overview
A cardiologist is a doctor who specializes in diagnosing and treating conditions which affect the heart. These may include high blood pressure, high cholesterol, coronary artery disease, heart attack, heart failure, or abnormal heart rhythms (arrhythmias).
The heart has a complex electrical system which causes the heart muscle to contract and pump blood through the heart and out to the body. It is important for the electrical signals to move through the heart cells in a coordinated manner to create a normal heartbeat and heart rhythm. If there is a problem with the heart’s electrical system, the heart does not function normally and a person may experience palpitations, weakness, lightheadedness, or may even pass out.
If you are suspected of having a problem with your heart’s electrical conduction system, your primary care provider or cardiologist may refer you to a cardiac electrophysiologist. An electrophysiologist is a cardiologist who has undergone additional training and is an expert in diagnosing and treating problems with the heart’s electrical system. They are trained to perform specialized electrophysiology tests and electrophysiology procedures.
What is electrophysiology?
Electrophysiology is the study of electrical impulses within cells and tissues. A cardiac electrophysiologist specializes in conditions which affect the electrophysiology of heart muscle cells.
Training and education
After approximately 8 years of undergraduate and medical school, a person completes at least 8 more years of medical training to become an electrophysiologist.
- Internal medicine residency. At least 3 years of formal, hands-on training in the care and management of health conditions in the adult population.
- Cardiology fellowship. Additional 3 years of clinical training in the care and management of diseases involving the heart. After completing a cardiology fellowship, a person is eligible to take a test to become a board-certified cardiologist.
- Electrophysiology fellowship. To become an electrophysiologist, a cardiologist completes an additional 2 years of subspecialty training in the care and management of health conditions affecting the heart’s electrical system. After the electrophysiology fellowship, a person must pass an exam to become a board-certified electrophysiologist.
What is electrophysiology used for?
Cardiac electrophysiology is used to diagnose and treat heart rhythm abnormalities (arrhythmias).
- Atrial fibrillation (AFib or AF). Arrhythmia caused by chaotic electrical impulses in the upper chambers of the heart (atria). AFib causes an irregular heartbeat and can be very fast. Atrial fibrillation increases the risk of blood clots in the heart and is associated with a 5 times increased risk of stroke. It can also lead to heart failure. Atrial fibrillation can be treated with medications and cardiac ablation.
- Atrial flutter. Arrhythmia which is similar to atrial fibrillation, but tends to be regular rather than chaotic. The treatment of atrial flutter is similar to that of AFib.
- Bradycardia. A normal heart rate is 60-100 beats per minute. Bradycardia is a heart rate less than 60 beats per minute. When a person has symptomatic bradycardia (i.e. tiredness, weakness, exercise/activity intolerance, lightheadedness, or passing out) a permanent pacemaker may be needed.
- Tachycardia. A heart rate above 100 beats per minute. An elevated heart rate can be a normal response to stress, infection, or physical exertion. However, if the heart rate is elevated without an appropriate cause, it may be due to a problem with the heart’s conduction system and may require treatment with medications or an electrophysiology procedure.
- Supraventricular tachycardia (SVT). An arrhythmia that originates in the atri. SVT causes the heart to beat too fast and can cause symptoms of palpitations. SVT can be treated with a cardioversion, medications, or an ablation procedure.
- Ventricular tachycardia. Arrhythmia that originates in the lower chambers of the heart (ventricles) which causes the heart to beat too fast. Unlike SVT, ventricular tachycardia can be dangerous and requires treatment, sometimes emergently.
- Ventricular fibrillation. Arrhythmia that causes the ventricles to quiver (fibrillate) and beat ineffectively. This is a life-threatening arrhythmia that can cause sudden cardiac death.
- Long QT syndrome. A condition which can increase the risk of the development of a very fast, potentially life-threatening arrhythmia.
- Wolff-Parkinson-White (WPW) syndrome. An abnormal electrical pathway in the heart that increases the risk of arrhythmia.
- Other cardiac arrhythmias. Electrophysiologists treat a variety of other arrhythmias.
What tests does an electrophysiologist do?
Electrophysiologists diagnose and treat abnormal electrical activity in the heart. In order to diagnose or treat an abnormal heart rhythm, an electrophysiologist may recommend some of the following tests:
- Electrocardiogram (EKG or ECG). This was the first electrophysiology test that allowed doctors to ‘see’ the electrical activity of their patients’ hearts. It was created in the late 1800/early 1900s and is still used today as the initial test for diagnosing an arrhythmia. An electrocardiogram is a quick, painless test that creates a tracing of the heart’s electrical activity and allows your doctor to see your heart rhythm and rate. The electrical activity in the heart creates characteristic waveforms on an electrocardiogram. Different abnormal heartbeats and arrhythmias create distinctive patterns of electrical activity on the EKG.
- Blood tests. Blood work will be done to check for issues that could contribute to a heart rhythm abnormality.
- Echocardiogram. An ultrasound of the heart. This test creates images of the heart and allows your electrophysiologist to see the size, structure and function of the heart.
- Holter monitor. Portable ECG monitoring device used to detect abnormal heartbeats and arrhythmias. It records the heart rhythm continuously for 24 hours or more.
- Event monitor. Portable ECG monitoring device similar to a Holter monitor. However, event monitors only record the heart rhythm when an abnormality is detected or when the person wearing the monitor has symptoms (i.e. palpitations, dizziness, etc.) and activates the monitor to record. Event monitors can be worn for up to 30 days.
- Implantable loop recorder. Small device that is implanted underneath the skin to the left of the breastbone. Device monitors for arrhythmias for up to 3 years.
- Stress test. A test that uses exercise or medication to stress the heart. During the test, your blood pressure and heart rhythm are monitored.
- Tilt table test. If a person has a history of passing out (syncope), a tilt table test may be recommended. The tilt table test tries to induce an episode of syncope in a controlled environment in an effort to determine the underlying cause. An automatic blood pressure cuff and cardiac monitor are used to monitor heart rate, rhythm and blood pressure throughout the test.
How does an electrophysiologist treat arrhythmias?
After an arrhythmia has been diagnosed, an electrophysiologist may recommend certain lifestyle changes, medications, or a specialized electrophysiology test or electrophysiology procedure to treat the abnormal heart rhythm.
Lifestyle changes
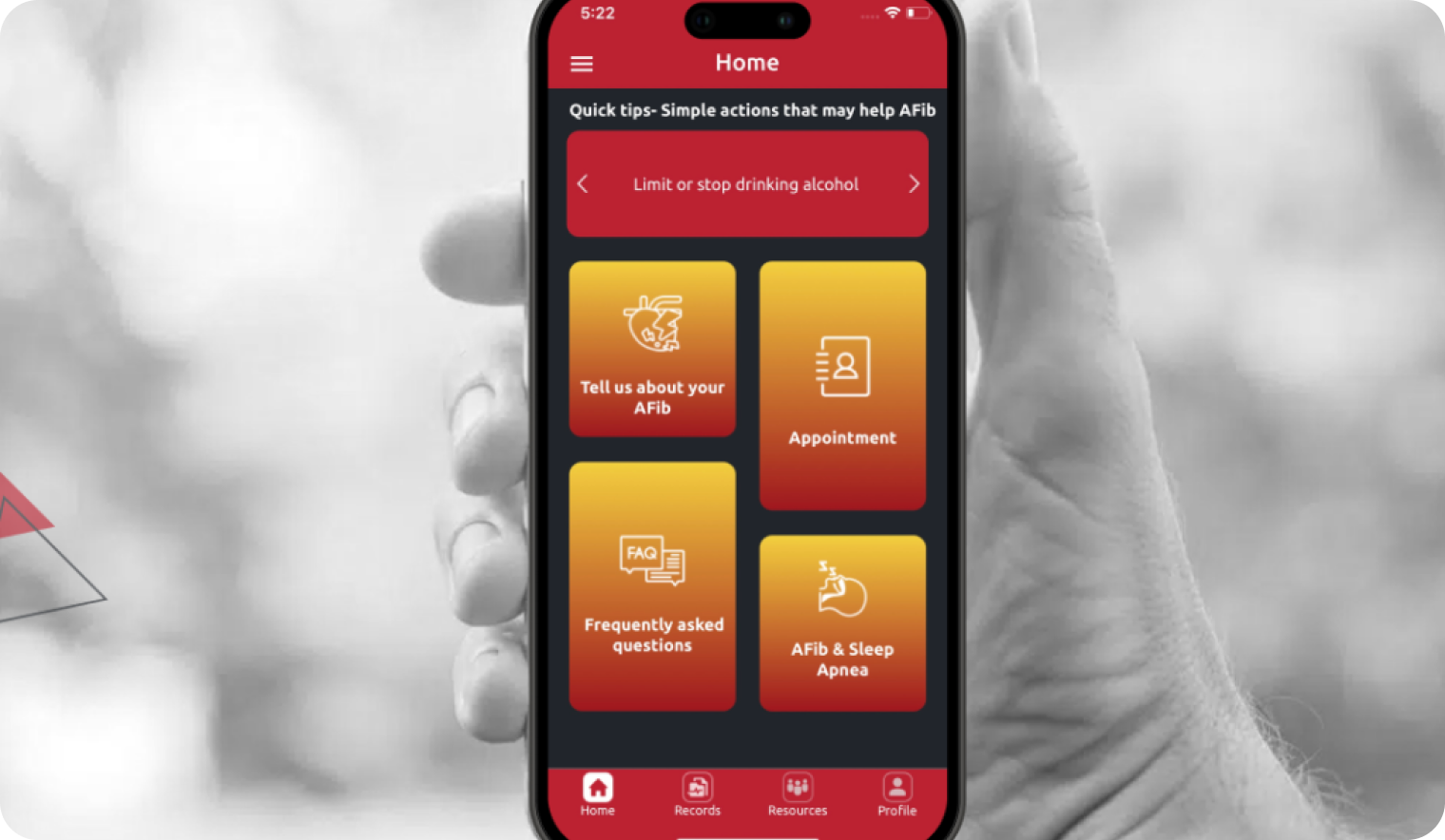
Some arrhythmias, like atrial fibrillation or atrial flutter, can be caused by modifiable risk factors like obesity, diabetes, heart disease, excessive alcohol intake and sleep apnea. Therefore, an electrophysiologist may recommend lifestyle changes like:
- Weight loss
- Regular, moderate–intensity physical activity
- Heart healthy diet
- Limiting alcohol and caffeine
- Quitting smoking
- Managing stress and anger
Medications
Medications may be used to control the elevated heart rate and abnormal heart rhythm associated with an arrhythmia. Medications may include beta-blockers or calcium channel blockers to control the heart rate. Antiarrhythmic medications help maintain a normal heart rhythm. When treating an arrhythmia, medications may be prescribed to be taken daily or on an as-needed basis.
Cardiac electrophysiology procedures
- Electrical cardioversion. Electricity is delivered to the heart to reset the heart to a normal rhythm.
- Electrophysiology study (EP study). Electrophysiology test performed in an electrophysiology laboratory. During an electrophysiology study, the electrophysiologist inserts a small flexible tube (catheter) into a blood vessel in the groin, arm or neck. The catheter is then guided into the heart. A specialized electrode catheter designed for the heart is used to locate the source of abnormal electrical signals and further define the type of arrhythmia. This process is called cardiac mapping. During an EP study, certain medications may be tested for effectiveness at suppressing abnormal electrical activity. The information gathered during an EP study also helps determine if an ablation procedure may be helpful in treating an arrhythmia.
- Catheter ablation. Electrophysiology procedure that uses heat (radiofrequency), freezing (cryoablation), or laser energy are used to create areas of scar tissue within the heart. This scar tissue interrupts the abnormal electrical signals that cause the arrhythmia. During an ablation, the electrophysiologist inserts a catheter into a blood vessel in the groin and guides the catheter into the heart. A specialized electrode catheter is used to locate abnormal electrical activity. These areas are then ablated using radiofrequency, cryoablation or laser energy. The specialized electrode catheter is then used again to verify that the abnormal electrical signals have been effectively blocked.
- Cardiac devices
- Pacemaker. Implanted device that prevents the heart from beating too slowly.
- Automatic internal cardiac defibrillator (AICD). Implanted device which is indicated for people with a history of cardiac arrest, sustained ventricular tachycardia or severe congestive heart failure. If an AICD detects ventricular tachycardia or ventricular fibrillation it can deliver an electrical shock to the heart to try to reset the heart to a normal rhythm.
- Biventricular pacemaker. Implanted device may be recommended for a person with advanced heart failure. A biventricular pacemaker helps the weakened heart muscle to beat in a more coordinated way and can help improve heart function.
When should you see an electrophysiologist?
If you have symptoms of palpitations, fluttering/pounding in the chest, dizziness, fainting, or an abnormal heart rhythm, your primary care provider or cardiologist may refer you to an electrophysiologist for an electrophysiology consult. The electrophysiologist can complete the highly specialized electrophysiology tests or cardiac electrophysiology procedures which may be needed to diagnose or treat abnormal heartbeats or an abnormal heart rhythm.
What to expect at an appointment with an electrophysiologist?
If you are referred for an electrophysiology consult there will be a lot of information to cover and limited time so it is helpful to be prepared. Know your medical history, family medical history and bring a complete list of medications. An electrocardiogram will probably be done during the visit and the electrophysiologist may order other tests to ensure an accurate diagnosis. If the diagnosis is already known, the electrophysiologist may prescribe new medications or recommend a procedure. The amount of information you receive can be overwhelming and sometimes it is helpful to take notes or bring a family member with you to the appointment. Be sure to bring a list of questions, starting with the most important questions in case there is not time to answer them all at the first appointment.