Maria is a 65 year old female who presents to the emergency room complaining of shortness of breath and palpitations. A heart monitor confirms the presence of an abnormal heart rhythm (arrhythmia) and shows atrial fibrillation (AFib) with a heart rate of 130 beats per minute. The nursing staff tell her the doctor will be in shortly to discuss the diagnosis of AFib with RVR (rapid ventricular response, meaning the heart rate is above 100 bpm). In the meantime, nursing interventions for atrial fibrillation are started. When the doctor comes in Maria asks him what caused the atrial fibrillation. He briefly explains the pathophysiology in AFib and tells her that her history of heart disease and heart failure probably contributed to her developing AFib.
What is the pathophysiology of atrial fibrillation?
Atrial fibrillation is a chaotic, irregular heart rhythm. It is the most common sustained arrhythmia seen in clinical practice. The prevalence of atrial fibrillation increases with age and is rare in people younger than 50 years. There are many medical conditions that increase the risk of AFib, some of the more common of which are hypertension, heart disease, diabetes, obesity, sleep apnea, thyroid disease, and heart failure. Smoking, excessive alcohol intake, and extreme endurance exercise can all also contribute to AFib. Caffeine’s impact on AFib is less clear with some studies showing increased AFib incidence with increased caffeine intake and others showing no effect.
The pathophysiology of atrial fibrillation is complex and is not entirely understood. Atrial fibrillation risk factors may contribute to the initiation or continuation of AFib by increasing systemic inflammation or changing the structure and function of the heart, particularly the left upper heart chamber (atrium). In addition, the autonomic nervous system and genetics may play a role in promoting AFib.
Here are definitions of some common terms used to describe AFib pathophysiology:
Trigger. A rapidly firing electrical focus that can initiate AFib. Over 90% of triggers for AFib are found within the pulmonary veins where they connect to the left atrium.
Substrate. The mechanical and anatomic structure within which atrial fibrillation can occur. Triggers initiate atrial fibrillation and the substrate maintains AFib.
Atrial remodeling. Changes in the heart’s electrical system or the mechanical and anatomic structure (substrate). These changes occur in the left atrium as a result of atrial fibrillation and AFib risk factors and increase the likelihood of AFib initiation and maintenance over time.
How is atrial fibrillation developed?
There are a number of factors which contribute to the development of atrial fibrillation. Medical conditions like hypertension, valvular heart disease, sleep apnea, and congestive heart failure apply mechanical stress on the heart and lead to structural and mechanical changes at the cellular level. These changes contribute to chronic atrial stretch and stiffening (fibrosis) of the left atrium. Risk factors also increase oxidative stress on the heart muscle cells (cardiomyocytes).
Atrial fibrillation may initially present as paroxysmal (self-terminates within 7 days) and eventually progress to persistent (continuous for greater than 7 days and up to 1 year) or long-standing persistent atrial fibrillation (lasting longer than 1 year). AFib is considered permanent if it is continuous and the patient and healthcare provider have decided against pursuing treatment options to restore and maintain a normal heart rhythm.
The triggers and substrate for atrial fibrillation develop over time. As remodeling occurs the probability of AFib progression from paroxysmal to persistent or permanent atrial fibrillation increases.
How does atrial fibrillation affect atrial function?
Normally, blood is pumped from the upper heart chambers (atria) to the lower heart chambers (ventricles) in a coordinated fashion. When the heart is in AFib, the atria quiver and lose their coordinated squeeze. This decreases their ability to move blood effectively to the ventricles.
Over time, atrial fibrillation also affects atrial function at the cellular level. Inflammation and oxidative stress lead to fibrosis, or stiffening, of the left atrium. The left atrium also tends to enlarge. A bigger and stiffer left atrium is even less effective at pumping blood to the ventricles.
How does atrial fibrillation affect cardiac output?
Cardiac output is the term used to describe how much blood your heart pumps each minute. The following equation is used to calculate cardiac output: stroke volume x heart rate = cardiac output. Stroke volume is the amount of blood the heart pumps with each beat. Heart rate is how many times the heart pumps per minute. A normal, healthy heart should pump 5 to 6 liters of blood per minute when a person is resting. In a healthy heart cardiac output increases with activity as a function of increased heart rate and stroke volume. This allows the heart to keep up with the increased oxygen demands of the muscles during exercise.
The chaotic, disorganized rhythm of atrial fibrillation affects what doctors call ‘atrial kick’. When a person is in atrial fibrillation, the coordinated contraction (squeeze) of the upper chambers is lost. Instead, the atria quiver which decreases the amount of blood that is pumped from the upper to lower heart chambers (ventricles) with each heartbeat. A healthy heart can compensate for this loss of atrial kick and in some cases can maintain stroke volume. However, that is not normally the case. Let’s look at an example in which a person has AFib with RVR with a heart rate of 145 beats per minute (bpm). One might think that the cardiac output would increase as the heart rate increases. However in atrial fibrillation, the irregular rhythm in the setting of a rapid heart rate and loss of atrial kick makes maintaining cardiac output difficult.
The loss of atrial kick means more time is required for the ventricles to fill with blood. But when the ventricular rate is high (i.e. 145 bpm, as in the example above) the ventricles don’t have as much time to fill. The loss of atrial kick compounds the problems because it slows down how quickly the atria are able to move blood to the ventricles. As the ventricles receive less blood and have less time to fill, the stroke volume will decrease.
Overtime, atrial fibrillation causes atrial remodeling which further decreases the ability of the atria to pump blood effectively. Atrial remodeling also makes maintaining a normal heart rhythm more difficult. As atrial fibrillation progresses from being paroxysmal to being persistent more substrate develops in the left atrium. When AFib is paroxysmal, almost all triggers are located in the pulmonary veins. However, as the substrate evolves through atrial remodeling AFib triggers develop within the substrate as well. At this point, treating atrial fibrillation becomes more complex. AFib ablation for paroxysmal atrial fibrillation can electrically isolate the pulmonary veins thereby preventing the electrical signals from AFib triggers from traveling into the left atrium to cause AFib. However, persistent AFib is more difficult to treat because the AFib triggers are no longer only within the pulmonary veins; they are also in the substrate throughout the left atrium.
Does AFib cause low oxygen levels?
Atrial fibrillation can make the heart beat too fast which can cause the heart muscle to weaken and lead to heart failure. When the heart muscle is weak it is unable to pump blood effectively out of the heart.
To better understand this it can be helpful to think of the heart as a bucket. Water (blood) is continually coming into the bucket (heart) and every second or so the bucket should empty about 50-70% of its water so it doesn’t overflow. Now imagine that the bucket is suddenly only able to pour off about 30% of its water but water keeps coming in at the same rate as it was before. What would happen to the bucket? It would overflow, right? This is what happens in heart failure.
Because the heart muscle is weak, every time the heart beats less blood gets pumped out of the left side of the heart than is coming into the heart on the right side. If you have more coming in than you have going out, you will always end up with overflow. When the heart ‘overflows’, blood backs up and fluid accumulates in the lungs, abdomen, and legs. Fluid accumulating in the lungs interferes with the lungs’ ability to oxygenate blood and for that oxygenated blood to get back to the heart to get out to the rest of the body.
What is the most common complication associated with atrial fibrillation?
Atrial fibrillation can lead to a number of complications including:
- Stroke. One of the most common serious complications of AFib is stroke. A person with atrial fibrillation has a five to six fold increased risk of stroke. This is because the chaotic rhythm of AFib can cause blood to pool in the left atrium. Pooled blood is more likely to form a clot (thrombus). If part of the clot breaks off and leaves the heart, it can be carried to the brain and cause a stroke. What are risk factors for AFib thromboembolism (i.e. a blood clot that forms in one area of the body and travels to another)? If you have atrial fibrillation, your doctor will use the CHA2DS2 VASc score to determine your risk of stroke. A higher CHA2DS2 VASc score means you have more risk factors for thromboembolism and thus a higher risk of stroke associated with your AFib.
C – Congestive heart failure (1 point)
H – Hypertension or high blood pressure (1 point)
A2 – Age greater than 75 years (2 points)
D – Diabetes mellitus (1 point
S2 – History of stroke, transient ischemic attack (i.e. mini-stroke), or thromboembolism (2 points)
V – Coronary artery disease, heart attack or peripheral arterial disease (1 point)
A – Age between 65 and 74 years (1 point)
Sc – Female Sex (1 point)
Stroke risk reduction is recommended for men with a CHA2DS2 VASc score of 2 or greater and women with a score of 3 or greater. Blood thinner medications (anticoagulation) is the most common form of stroke risk reduction. However, if you are unable to take an anticoagulant, there are also procedures which can decrease stroke risk.
- Heart failure. Another common complication of AFib is heart failure (cardiomyopathy). Atrial fibrillation can either cause the heart muscle to become weak or it can make an already weak heart muscle worse. What is AFib cardiomyopathy? AFib causes the heart to beat too fast which can lead to tachycardia-mediated cardiomyopathy. This is when the fast heart rate (tachycardia) weakens the heart muscle so it is unable to move blood through the heart effectively. This can lead to fluid backing up into the lungs, abdomen, and legs. If a person has cardiomyopathy secondary to AFib, medications or electrical cardioversion can be used to revert the heart back to a normal rhythm. Ideally, after the stress of atrial fibrillation and tachycardia are removed, the heart function returns to normal.
- Heart attack (myocardial infarction). AFib is associated with an increased risk of heart attack; especially amongst women and African Americans and in the first year after AFib diagnosis.
- Memory loss or cognitive impairment. There is a higher rate of dementia amongst people with AFib. This may be related to the increased risk of stroke.
- Blood clots. In addition to an increased risk of stroke, people who experience thromboembolism associated with atrial fibrillation can have blood clots that embolize and affect the lungs, kidneys, spleen, and intestines.
What is atrial fibrillation nursing?
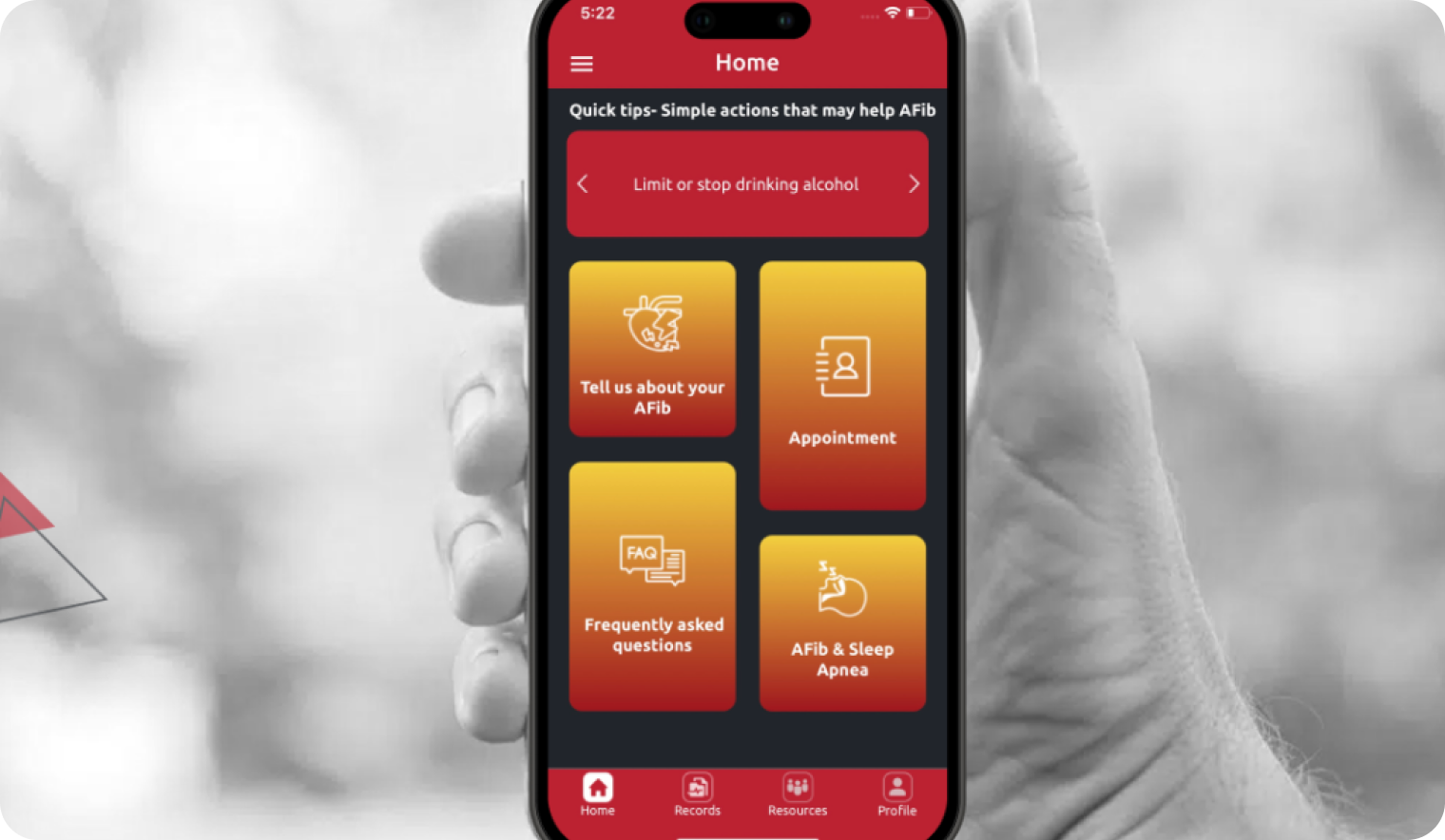
Atrial fibrillation is a complex disease. Medical therapy in atrial fibrillation involves lowering the heart rate, restoring a normal rhythm, and stroke prevention. Medications, cardioversion, ablation, or other procedures are all options for the treatment of atrial fibrillation. Another vital part of AFib treatment is the evaluation and management of AFib risk factors which may involve additional medications and also often requires lifestyle changes.
Multiple studies have demonstrated improved outcomes for patients with atrial fibrillation whose care is managed by a medical team. In the team approach, patients receive more individualized care and closer follow-up. AFib teams often include a cardiologist or electrophysiologist, primary care provider, nursing staff, a pharmacist, and, perhaps, an exercise physiologist. Each team member uses their expertise to support the patient through the AFib process.